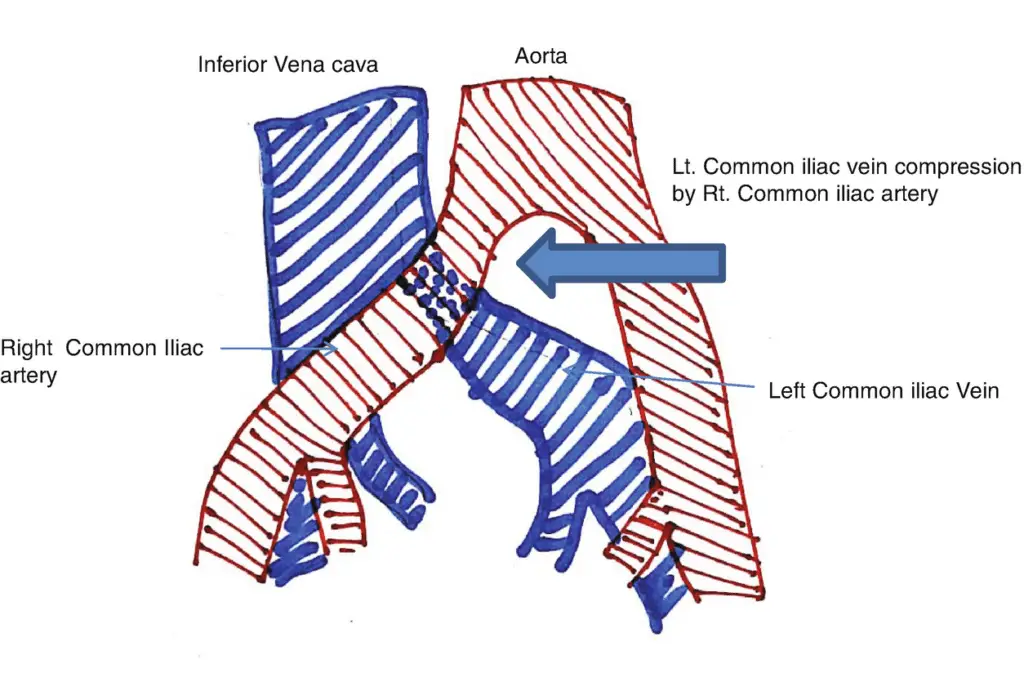
May-Thurner syndrome is a condition caused when the left iliac vein in your pelvis is compressed by the right iliac artery. In other words your left iliac vein arrows down due to pressure applied by the right iliac artery in your pelvis.
Some other common names used for May-Thurner syndrome are:
Cockett syndrome
Iliocaval compression syndrome.
Iliac vein compression syndrome
Due to the pressure applied, the risk of DVT or deep vein thrombosis increased in the left extremity. DVT is a type of blood clot that may either completely or partially block the blood flow through your veins causing complications.
Left iliac main is the most important and main vein present in your left leg. Its function is to carry blood from your heart back to the legs. The right iliac artery is the vein artery of your right leg that delivers the blood to your right leg. Complications in either of these veins or arteries can be harmful.
The right iliac artery sometimes is present on top of the left iliac vein causing pressure on it thus leading to the may-Thurner syndrome. There may be serious consequences of the pressure applied.
This article lets you know the causes, symptoms, and treatment options for the may-Thurner syndrome.
Different symptoms of the May-Thurner syndrome
May-Thurner syndrome is present in many people but it is not associated with any complication unless it turns into DVT or deep vein thrombosis. Some people might face certain symptoms without even DVT due to difficulty in normal circulation of the blood from the heart to the leg.
Some must-know symptoms you can consider in the left leg predominantly include the following
Leg swelling
Pain in leg
Your leg starts feeling heavy
Pain in the leg while you try to walk
Discoloration of the skin due to no blood supply
Ulcers in leg
Veins of the leg become enlarged
These symptoms can occur without DVT too but if you have DVT along with may thunder syndrome you may suffer from additional symptoms like leg pain, throbbing or tenderness in the leg, skin turning red and warm to touch, etc. All other symptoms of DVT are the same as May-Thurner syndrome.
If you anyhow experience these symptoms or the pain becomes intolerable, you must see a doctor to find out the possible cause and underlying conditions behind May-Thurner syndrome if any.
Causes of the May-Thurner syndrome
As you have already read in the overview, this syndrome occurs when pressure is applied by the right iliac artery on the left iliac vein present in the pelvis. However, it is unfortunate to note that many details are not still available on the causes of the right iliac artery putting pressure on the left iliac vein.
It is difficult to know the reason behind having may Thurner syndrome because most of the time it occurs without causing symptoms of pain.
However, as per a study conducted back in 2015, It was found that only 2 to 3 percent of individuals developing DVT can connect it to the may-Thurner syndrome.
According to another study from 2018, it was found that the frequency of occurrence of the may-Thurner syndrome in women is twice as often when compared to that in men. In addition to these facts, may-Thurner syndrome mostly occurs in people between the age groups of 20 to 40. This was reported in a study and review in 2013.
Risk Factors Associated with the May-Thurner syndrome
Certain risk factors may increase the risk of deep vein thrombosis in patients of the may-Thurner syndrome. These risk factors include- usage of birth control pills, cancer, infection, dehydration, pregnancy, prolonged activity, etc
Before it’s too late and the chances of DVT increase, you must get it diagnosed in the initial stages for better and fast treatment. Let’s see what are different diagnosis options available for may-Thurner syndrome.
Diagnosis of May-Thurner syndrome
You already know by now that the symptoms of may thunder syndrome are normal and are the same as an injury so it becomes slightly difficult for doctors and healthcare providers to diagnose if it is DVT and May-Thurner causing pain.
Most healthcare providers begin by asking you your medical history and reports. You might have to go through some physical examinations for a complete diagnosis. Doctors reply on imaging tests too if the left iliac vein is narrowed by the right iliac artery in the right leg.
Either invasive or non-invasive approaches are utilized to diagnose.
Here are some non-invasive as well as invasive tests your health care provider may ask you to participate in:
Invasive tests include catheter-based venogram and intravascular ultrasound using a catheter for performing ultrasound from the inside portion of the blood vessels.
Non-invasive processes are also reliable and these include venograms, MRI scans, CT scans, and ultrasound.
If the diagnosis is missed in the younger population, recurrence of deep vein thrombosis may lead to postthrombotic syndrome further causing mortality and morbidity. The key to successful treatment is early diagnosis as this will help fix anatomical lesions along with the use of anticoagulation and removal of clots.
May-Thurner syndrome without a clot
Patients who do not develop deep vein thrombosis or blood clots in association with the may-Thurner syndrome do not face symptoms most of the time. In this case, the narrowing of the vein can be discovered easily using CT scans and normal procedures. There are very few chances of varicose veins, venous claudication, and venous stasis ulcers in this scenario.
Treatment options for May-Thurner syndrome
This syndrome is caused due to reduced blood flow in the left iliac vein after it is narrowed down so the treatment options included a focus on improving the blood flow in the iliac vein. The treatments involved not only help get relief from the symptoms but also lowers the risk of acquiring deep vein thrombosis in affiliation to the may-Thurner syndrome.
There are certain ways through which pain can be relieved with increased blood flow. These include:
Bypass surgery- This treatment focuses on rerouting the blood around the compressed regions of left iliac veins with a bypass graft.
Angioplasty and stenting- In this treatment, a small catheter is inserted into the veins with a balloon on the tip and then this balloon is inflated for opening the narrowed veins. A small mesh tube is also used known as Stent for keeping the vein opened. Later the balloon inserted is deflated and removed but the stent remains in place.
Repositioning the right iliac artery- Instead of performing procedures on the left iliac vein, in this treatment the right iliac artery is repositioned and moved behind the left iliac vein to remove its pressure.
Anticoagulation- It is the same as having blood thinners to prevent clotting of blood. You may be referred to an anticoagulation clinic to offer this treatment. Your physician or healthcare provider may monitor you closely when you take blood-thinning medications to avoid risk factors.
In case the may-Thurner syndrome further leads to Deep vein thrombosis, some extra precautions are taken by the doctor with additional treatments to treat both conditions.
If you are suffering from DVT along with or due to may-Thurner syndrome, the following treatments may be used-
A vena cava filter- This filter is designed to prevent blood clots from reaching your lungs. This procedure uses a catheter inserted inside the vein of the groin or neck and then inside the inferior vena cava. This filter is specifically made to catch the clots so that they do not reach your lungs. However, it cannot stop the formation of new clots which require some other treatments.
Clot-busting medications- Clot-busting medications can be inserted into your body via a catheter which helps to break new clots. It nearly takes from hours to days for these clots to dissolve and get rid of.
Blood thinners- These are certain medicines and drugs used to prevent clotting of blood thus preventing Deep vein thrombosis.
Despite these treatment options, the may-Thurner syndrome might cause certain complications. When the blood clots inside your left ruptures or breaks, it becomes free to travel through the bloodstream. This makes it free to reach other organs such as your lungs causing a blockage called Pulmonary embolism. This is a fatal or life-threatening condition requiring immediate medical attention. If you experience shortness of breathing, chest pain, or coughing up a mixture of mucus and blood, you must call your doctors immediately and seek treatment as soon as possible.
Know that some of the treatment options do include surgical procedures to treat may-Thurner syndrome and DVT. Some surgeries are performed on an outpatient basis which means you will be discharged immediately after the surgery gets over. You should be able to get back to your regular activities within a few days to mostly a week.
However, bypass surgery still requires some rest and you might have soreness afterward. It might take a few weeks or even months to make a complete recovery. Always ask questions and take instructions from your healthcare provider on follow-ups. If the stent is used in your process you will be asked to visit every week for an ultrasound. Make sure you do not miss these appointments to reduce the risks of complications in procedures.
The Bottom Line
You must know that having May-Thurner syndrome should not sound panicking to you because many people have this life long without requiring treatment and without even knowing it. If you witness signs of pain or swelling now and then, you must visit a doctor. If it leads to deep vein thrombosis or you notice any symptoms of pulmonary embolism, that is the time when it requires immediate treatment.
If there is a chronic may-Thurner syndrome, make an appointment with sliced doctors and mention your concerns. They will help you with diagnosis and early treatment to avoid life-threatening complications later.
References:
https://www.cureus.com/articles/17188-clot-mayhem-a-case-of-may-thurner-syndrome
https://www.wjgnet.com/1949-8470/full/v7/i11/375.htm
https://www.ahajournals.org/doi/pdf/10.1161/circulationaha.115.019944 (aha journals)
https://journals.sagepub.com/doi/10.1177/1358863X18794276
