Wondering what is bacterial vaginosis (BV) and how it happens? Bacterial vaginosis is a common infection that occurs due to the growth of normal bacteria that resides in the vagina—changes in the average balance of bacteria in the vagina cause BV.
Bacterial vaginosis does not cause other health issues, but it may lead to problems, particularly when getting pregnant.
Here’s all you need to know about bacterial vaginosis and its symptoms, cause, and treatments.
What is bacterial vaginosis?
Bacterial vaginosis is an infection in the vagina caused by certain bacteria. It is the most well-known cause of unusual vaginal discharge in women of reproductive ages (women who still have their menstrual cycles and have not gone through the menopause phase).
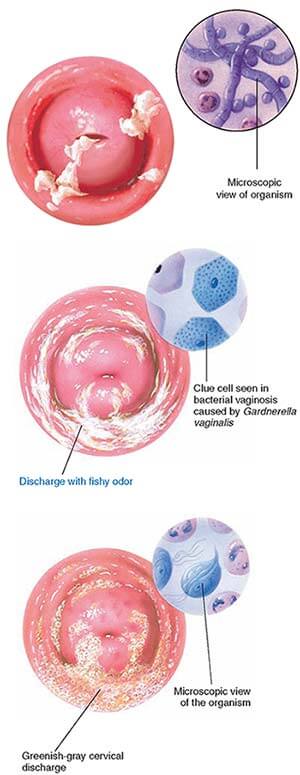
Bacterial vaginosis might result in a “fishy” odor and lead to vaginal irritation in a few women. Some women, on the other hand, might not have any symptoms at all.
Bacterial vaginosis is linked to poor gynecologic and obstetrics results like preterm delivery and disease after surgeries like hysterectomy. It might make a woman more receptive to sexually transmitted infections (STDs), particularly HIV.
Bacterial vaginosis is the most prevalent vaginal issue in ages 15 to 44 (menstrual cycle). An approximated one in three women in the United States will get Bacterial Vaginosis. The rate is estimated to be higher in black women.
Who can acquire bacterial vaginosis?
Wondering if you can get bacterial vaginosis or not? Anyone having a vagina might get bacterial vaginosis. It does not matter if you have had sex or not. But that is highly rare. It typically happens in women who are active sexually. You might have a more prominent risk of having Bacterial Vaginosis if you have the following:
- You are pregnant.
- You do not use dental dams or condoms.
- You have an intrauterine device (IUD).
- You have various sex partners.
- You have sex with a new partner.
- You have a female sex partner.
- You use douches.
Douching usually bothers the natural stability and balance of bacteria. Also, the balance of bacteria can be disturbed with the usage of scented soaps, vaginal deodorants, and bubble baths.
Having a new sex partner, or more than one partner, also makes it much more likely to acquire Bacterial Vaginosis. It is not yet clear why, but it has been observed that women having female partners are more likely to be at risk. You may get BV from anal and oral sex as well.
The Intra-Uterine birth control device, which is placed inside the uterus, has been associated with BV, particularly if you have abnormal menstrual bleeding. But it is not yet clear whether it is a primary cause or not. Note that you cannot get vaginal contaminations like BV from using swimming pools or standard toilet seats.
Causes of bacterial vaginosis
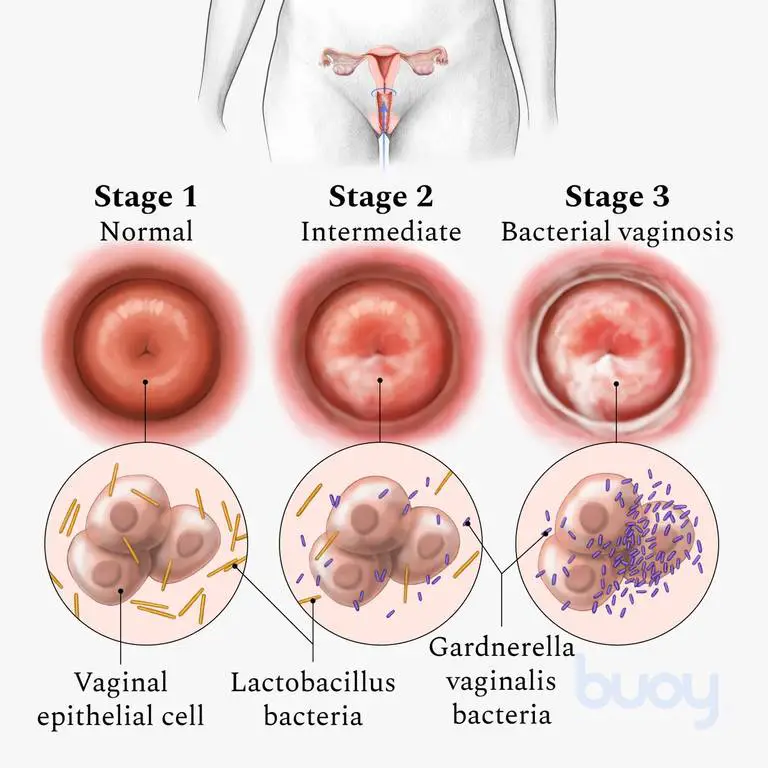
Your vagina is known to be home to various kinds of bacteria (therefore known as a microbiome), similar to the digestive system. Bacterial vaginosis occurs when some of the bacteria in your vagina grow more speedily than others. An excessive number of one type of bacteria will lead to a disproportion in the number.
A different type of bacteria known as lactobacillus keeps the vagina somewhat acidic so that harmful bacteria do not develop well. If the levels of lactobacillus drop, harmful bacteria start to move in, and you acquire Bacterial Vaginosis.
Symptoms of bacterial vaginosis
Nearly half of the time, women dealing with Bacterial Vaginosis have none of the symptoms given above. But they may include:
- Burning feeling during you pee
- A fishy odor that gets more powerful after sex
- Itching
- Thin green, gray, or white discharge
It is not similar to a yeast infection. Yeast infections often possess a thick white release that does not smell.
Diagnosis of bacterial vaginosis
The doctor will:
- Question about the medical history of patients.
- They will conduct a comprehensive physical exam.
- Perform a pelvic exam
- Monitor your vagina’s pH and acidity level.
- Take a small sample of discharge from the vagina to study for cells incorporated with bacteria.
Treatment of bacterial vaginosis
The doctor might order some antibiotics such as metronidazole, clindamycin, and tinidazole to handle Bacterial Vaginosis. That can be the medicine you take orally or a cosmetic or gel you dab onto the vagina. You will want to take most medications or gels for 5 to 7 days. Complete all the medicine suggested by the doctor, even if the signs of infection go away. If you finish early, there are chances of infection coming back.
Considering Bacterial Vaginosis can be developed through sex, make sure not to have sexual contact until you take medicine and the symptoms are completely gone. If your companion is a woman, they might need to see the doctor as well to find out if they require treatment.
Even after Bacterial Vaginosis is cured and goes away, it frequently returns. If that occurs, you will most likely require to take antibiotics repeatedly for a prolonged time.
If you are using an Intra Uterine Devise, and Bacterial Vaginosis seems to keep coming back (repeated BV), you might need to discuss another kind of birth control method with the doctor.
Prevention of bacterial vaginosis
You already know that bacterial vaginosis (BV) is not thoroughly understood by doctors. There aren’t any dependable ways of withdrawing from it. However, These steps might help lessen your risk of getting BV:
-
- Prevent douching – It alters the average balance of bacteria inside the vagina. Alternatively, follow healthy vaginal or vulvar care.
- Avoid vaginal connection with anything that has come in contact with your anus – Few things like sex toys and toilet paper might transport bacteria inside your poop to the vagina. Ensure that the sex toys you use are correctly sanitized after every use.
- Limit the number of sex partners you have – Analysis shows you are more likely to develop Bacterial Vaginosis if you have more than one or two sex partners.
- Use dental gums or latex condoms – Although it is not yet clear why the study reveals that sexual activity is linked to Bacterial Vaginosis.
- Wear cotton-lined or cotton lingerie – Bacteria flourish in moist conditions. Cotton supports in absorbing any moisture.
Usually, one course of antibiotics — used for up to seven days — helps you get rid of the infection. Approximately 10% to 15% of women need an extra round of treatment for eliminating vaginosis. Nearly 80% of women might get bacterial vaginosis repeatedly.
Are there complications in bacterial vaginosis?
Bacterial vaginosis has been linked to a more uplifted risk of different health predicaments, these include:
- A bacterial disease, if you had had a hysterectomy or any other operation on the female organs when dealing with bacterial vaginosis.
- A low birth or premature weight baby.
- Sexually transmitted diseases (STDs) like gonorrhea, chlamydia, herpes, or transferring HIV to your companion.
- Less benefit with fertility procedures like in vitro fertilization (IVF)
- Pelvic inflammatory disease or PID occurs in your ovaries, fallopian tubes, and uterus.
When to see a doctor?
Because Bacterial Vaginosis symptoms may look like those from yeast infection or other infections, it is crucial to find out the root cause of vaginosis. See your healthcare provider if you:
- Have an unusual vaginal discharge with a stink or a fever
- Have multiple intimate partners or a different partner (You may need to be examined for an STD or sexually transmitted disease as well)
- Used an over-the-counter medication to treat yeast infection but still beget symptoms.
References:
https://www.mayoclinic.org/diseases-conditions/bacterial-vaginosis/symptoms-causes/syc-20352279
https://www.womenshealth.gov/a-z-topics/bacterial-vaginosis
https://my.clevelandclinic.org/health/diseases/3963-bacterial-vaginosis
